Let’s be honest and address patient experience of A&E

Urgent and emergency care services continue to be under intense pressure. This is reflected in recent national data, showing a record number of patients having to wait more than 12 hours in accident and emergency last year. This is also reflected in the stories we receive from people, with positive experiences of A&E services falling.
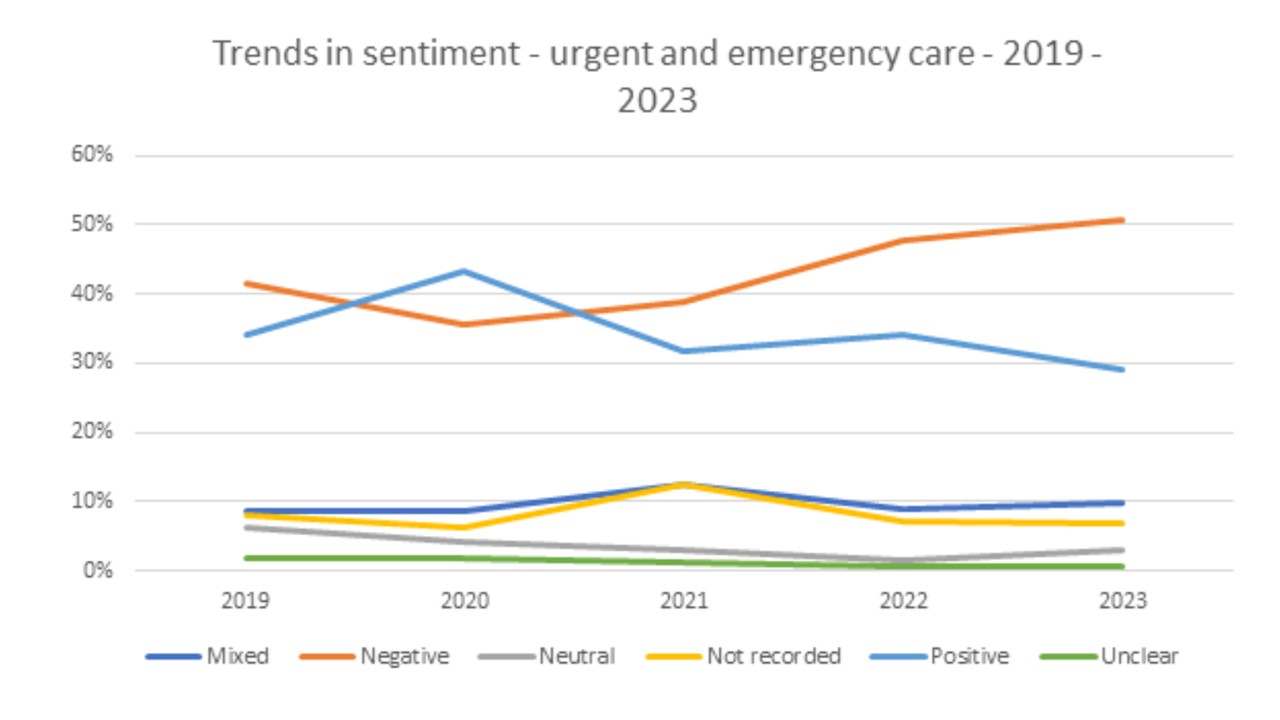
Of nearly 10,000 feedback pieces related to urgent and emergency care we received over the last five years, negative experiences of A&E increased by 23 per cent, from 42 per cent in 2019 to 53 per cent in 2023.
Our in-depth analysis of 789 stories received in November showed people waited to be seen in A&E between three and 27 hours. While we heard of pleasant waiting rooms with kind, patient, and supportive staff, it was often the opposite for many people.
Long waiting times were compounded by overcrowded, overly warm and uncomfortable conditions, with people lying on the floor, perching on radiators, with limited or unhygienic toilets, and little food and drink. In one extreme case, a waiting room resembled a treatment area, with people lying on the floor, on drips, while an older person who had a broken hip sat in a chair for two days without food.
“Absolutely shocking. The waiting room is in fact a treatment area. People laid on the floors on drips for days. Extremely poorly people ignored. Patients caring for patients as no one else to care for them. Elderly with broken hips sat in chairs for two or three days often not given a sandwich as they don't speak up. Patients shouted at should they fall off a chair. Waiting area not cleaned in days of sat there as floor covered in people.” Story shared with Healthwatch England
We also heard about A&E staff who went the extra mile for people, with patients recognising that staff are under extreme pressure
“Despite the long wait at times, every nurse, doctor and technician was patient, positive, and friendly. At any one time while I was there (17:30-23:30), there seemed to be 30-50 patients, plus family, friends, etc, which explains why it's busy.” Story shared by Healthwatch Harrow
Poor experiences in A&E are unfortunately not new; in fact, many are the same as those reported five years ago. However, we’re yet to see tangible action to address them.
Mapping a return to the more ambitious 95 per cent A&E target will help decision makers understand the scale of current challenges and the level of support needed. But targets alone won’t fix everything. Our evidence shows that there are other factors that matter to patients, such as how quickly they are initially triaged, their access to food, water, and pain relief, and the quality of communication while waiting for care.
Improving waiting room conditions
Waiting rooms can often be extremely busy and crowded, with frustrations experienced by patients and staff alike. But ensuring patients feel safe and comfortable at a time when they will be anxious and nervous about their health is vital.
This includes making waiting rooms accessible for those with access needs, giving people the privacy to discuss their condition, keeping patients informed about how long they may be expected to wait, and making sure waiting areas and toilet facilities are kept clean. Information screens and access to Wi-Fi and electrical charging points could also make waiting as comfortable as possible for patients.
Some of these issues are understood through data, such as the Care Quality Commission’s Urgent and Emergency Care Survey. However, this is only published every two years.
Alongside this collection, hospital departments should do more in real time to understand people’s personal needs in waiting rooms. And crucially, services need to act on this feedback to drive improvements.
Much of this data is already collected through local initiatives or the friends and family test, where follow-up questions in particular can provide A&E departments with key feedback to learn what matters to their patients while waiting. This data, however, is not used, with the only part reported being the headline satisfaction figure.
Moving closer to real-time data collection and reporting will help departments to get under the hood of patient experience, moving beyond satisfaction measures to address concerns, especially from the most vulnerable people, and encourage a culture of listening and learning.
The crisis in A&E is not an isolated problem. We also need to see solutions to workforce challenges and hospital discharge delays, investment in social care, and promotion of the NHS 111 scheme so patients can be pre-booked into GP or A&E slots and receive more consistent clinical advice over the phone.
This system-wide approach, alongside ambitious targets and a better understanding of what matters to patients, is key to supporting A&E teams to better care.
This system-wide approach, alongside ambitious targets and a better understanding of what matters to patients, is key to supporting A&E teams to better care.
Our recommendations
- A longer-term plan for reducing waiting times, including a focus on the longest waits, particularly for vulnerable patients. This should include mapping a return to the previous target of 95% of all patients being seen in four hours in A&E, as the current target of 76% can hide the scale of challenges facing teams and may put too many people at risk of being seen too late, or experiencing over-crowded waiting rooms.
- Better processes and patient journeys through hospital, via improved discharge processes, investment in social care, and promotion of the NHS 111 scheme so that patients can be pre-booked into GP or A&E slots and receive more consistent clinical advice over the phone.
- Real-time data collection and reporting on patient experience in A&E. Alongside clinical targets, we need to gain a deeper understanding of what matters to patients, including how quickly they are initially triaged, their access to food, water and pain relief, and the quality of communication while waiting for care. We want to see A&E departments formally review and report on lessons from follow-up questions in the friends and family test, as well as headline satisfaction measures.
The original blog was published in Health Service Journal on 6 February.


