Referrals: improving experiences and closing “black holes”

In 2023, we researched how difficult the process of getting a referral can be. People described how they ended up trapped in “referral black holes”, left without updates about their care.
In this follow-up report, we look at whether experiences of referrals have improved, and make recommendations to ensure referral processes work for patients and NHS teams alike.
Background
Since our last research, there have been national changes to referrals. These include more visibility of referral journeys through the NHS App, pharmacy referral pilots for suspected cancer and a greater drive to increase referrals into community rather than specialist services.
There’s evidence that some of these changes are already having a positive effect, while others carry risks. We’ve also continued to hear from people who feel forgotten throughout the referral process.
Our key findings
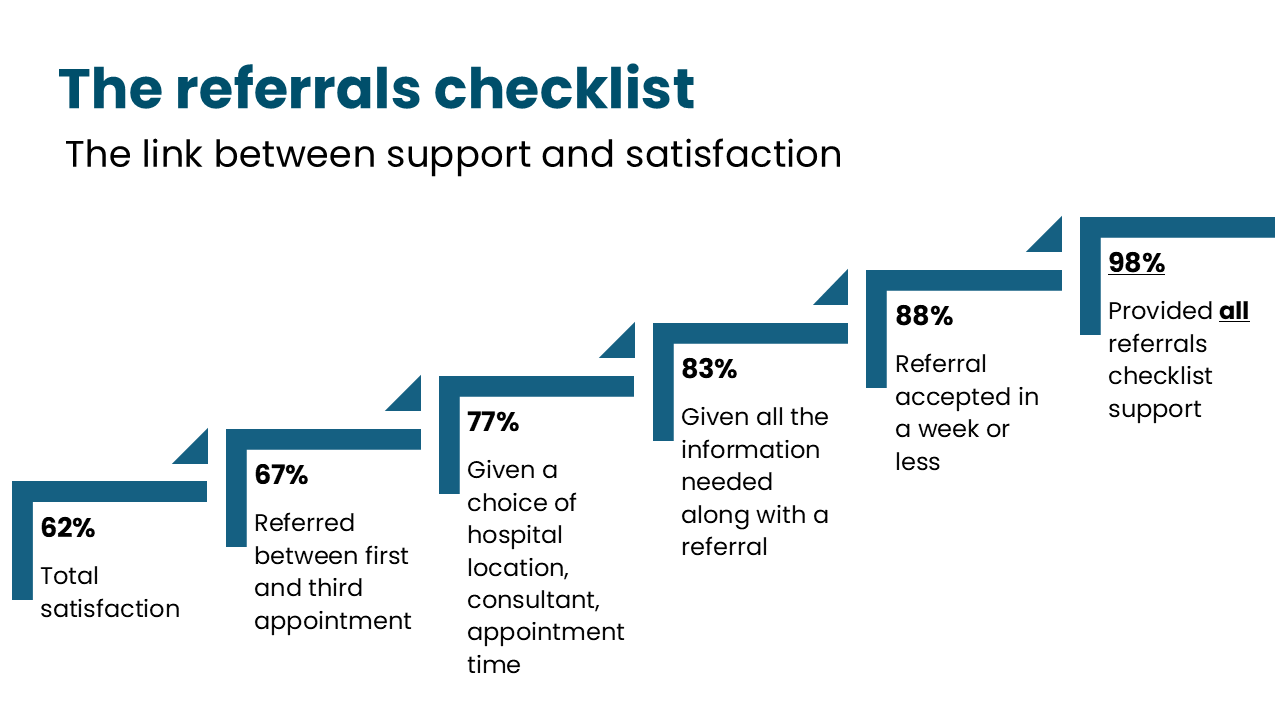
Over six in ten (62%) were satisfied with the referrals process. But almost one in four (23%) weren’t satisfied, and only 7% of those experiencing a referral issue were satisfied with the process.
One in seven (14%) people ended up in a ‘referral black hole’ – i.e. their referral is delayed, lost, rejected, or not sent. Three in four people (75%) who had an issue with their referral reported at least one negative impact on their health and wellbeing, compared with 36% of those who had no referral issues.
Earlier referral leads to better experiences. Of the 59% of respondents referred during their first GP appointment, 71% went on to be satisfied with the referral process. Satisfaction was 67% when people were referred between their first and third appointment. Only 47% of those needing more than three appointments were satisfied with the overall process.
Quicker referral confirmation leads to better experiences. People who had referrals confirmed within a month were significantly more likely to report satisfaction with the referral process. For those confirmed within a week, satisfaction was high at 88%.
The right information and choices lead to better experiences. Satisfaction rose to 83% when people got all the information they needed along with a referral. Satisfaction also jumped from 62% to 77% when given any sort of choice (e.g. of location, consultant, or appointment time) at the point people were told they were being referred.
Regular updates and support after referrals lead to better experiences. Nearly half (47%) said clear communication was among their top three important aspects of a referral. Regular communications after referral increased satisfaction.
Earlier referral with quicker confirmation and better information and choice leads to almost universal satisfaction. Satisfaction rose to 98% for those who were referred between their first and third GP appointment, had their referral confirmed within a week, said they were given enough information, and were given choices.
Our key recommendations
The NHS should introduce a referrals checklist with clearly marked responsibilities for different NHS teams. Our research clearly shows what makes or hampers a good referral experience. The upcoming NHS minimum standards for elective care should reflect this with resources for NHS staff to deliver the care people need.
Elective minimum standards must be expanded to cover all referral pathways. Currently, the standards are planned to help those referred for non-urgent elective pathways. To ensure consistency, these standards should cover other pathways too, including cancer, mental health, and neighbourhood referrals.
The 10 Year Workforce Plan must invest in trained admin staff to support people’s referrals journeys. The elective reform plan promises more training for non-clinical staff. But there must be more recruitment, training and support of administrators, navigators and coordinators to support better delivery of patient communications and updates.
Jess’ Rule must be implemented quickly and consistently. The recently announced rule encourages GP teams to consider second opinions or referral after someone has three appointments for the same unresolved health issue. There must be support alongside this to help teams meet potentially increased demand and waiting list support.
Downloads
Our report is also available in Easy Read and Large Print. If you need this report in a different format, please email enquiries@healthwatch.co.uk or call 030000 68 3000

