What are people's experiences of urgent and emergency care?

The pressure on urgent and emergency care services has been a big story recently, with significant press coverage of ambulance delays and long waits in accident and emergency departments (A&E).
This is backed up by the official performance statistics, which paint a grim picture as we head into winter.
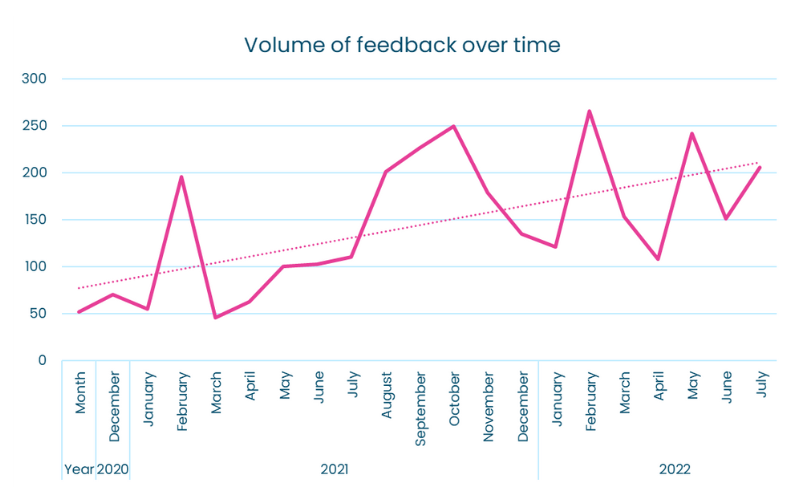
To understand how the pressures have affected patients, we looked back at the experiences of urgent and emergency care services people shared with us between December 2020 and August 2022.
More than 3,000 people gave us feedback, and the number of cases shared grew over time.
Nearly half (49%) of this organic feedback was negative. This is broadly in line with other areas of care we monitor. However, particular themes in the feedback showed new concerns around waiting times.
To help the NHS better prepare for the difficult months ahead, we wanted to test out whether the views of the public reflected the experiences shared with us.
In August 2022, we worked with Survation to ask a nationally representative sample of 2,036 people their thoughts on urgent and emergency care services.
We asked whether they had used services such as A&E, ambulances, and NHS 111, if they were confident that these services could offer timely and effective care and whether this confidence had changed over the pandemic.
Highlights from the polling
The key themes identified from our polling included:
- People feel confident that they will receive high-quality care from urgent and emergency services, but believe they will have to wait a long time to receive it.
- People's confidence in services changed throughout the pandemic.
- Those who were admitted to hospital following a visit to A&E were more likely to say their confidence in the service had increased.
- Older people have lower level of confidence in urgent and emergency services.
People are confident they will receive high-quality care but think they'll have to wait for it
"The staff and the NHS are amazing but so stretched -running from patient to patient. The young doctor who saw me had only had three hours sleep since Tuesday -he was doing 12 hour shifts and covering for all other staff that were off.”
Story shared with Healthwatch Dorset, June 2021.
We asked people to rate how much they agreed with the statements about urgent and emergency care services.
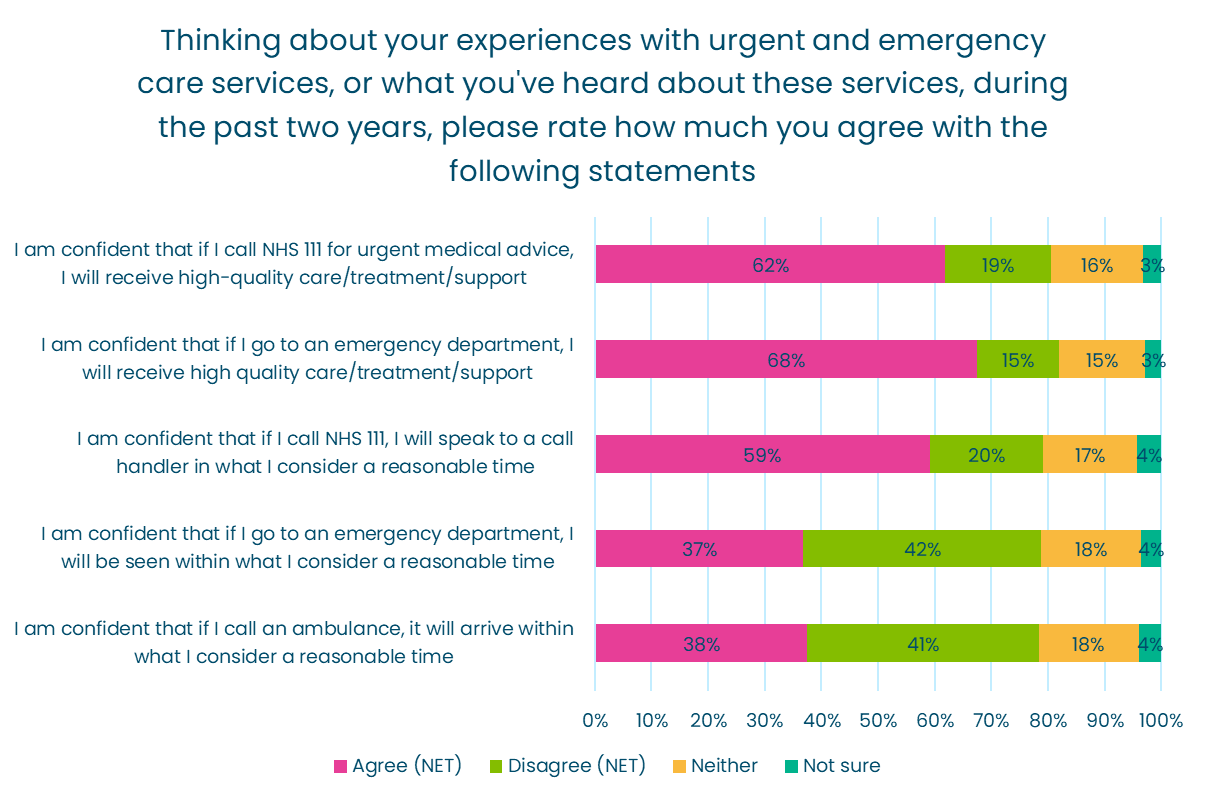
- Nearly two-thirds of people agreed that they were confident they would receive high-quality care, treatment or support at an emergency department such as A&E or a minor injury unit.
- However, people were not confident that ambulances would arrive in a timely fashion nor that they would be seen in a reasonable time in an emergency department. Just three in eight people we asked said they felt they would be seen in a reasonable time at an emergency department or that an ambulance would arrive in a reasonable time.
People’s confidence has changed as a result of the pandemic
We asked people whether their overall confidence in urgent and emergency care services had changed throughout the pandemic:
- Over half (58%) of people agreed that their confidence had changed over the pandemic, compared to 23% who said it had not and 19% who were unsure.
- It had overwhelmingly fallen for those who told us their confidence had changed. 72% of the people who said their confidence had changed said it had decreased.
- Just a quarter of people whose confidence had changed said it had increased over the course of the pandemic.
- Our data also indicates that stories about urgent and emergency care services in the media are a key driver of people’s change in confidence. 30% of people whose confidence had changed told us it was due to television, radio, or newspaper stories.
However, we can also see that personal experience influences confidence. 20% of the people whose confidence changed said it was due to their experience of urgent and emergency care services, and 21% said their confidence change was due to the experience of someone they knew.
Those admitted to hospital following a visit to A&E were more likely to say their confidence had increased
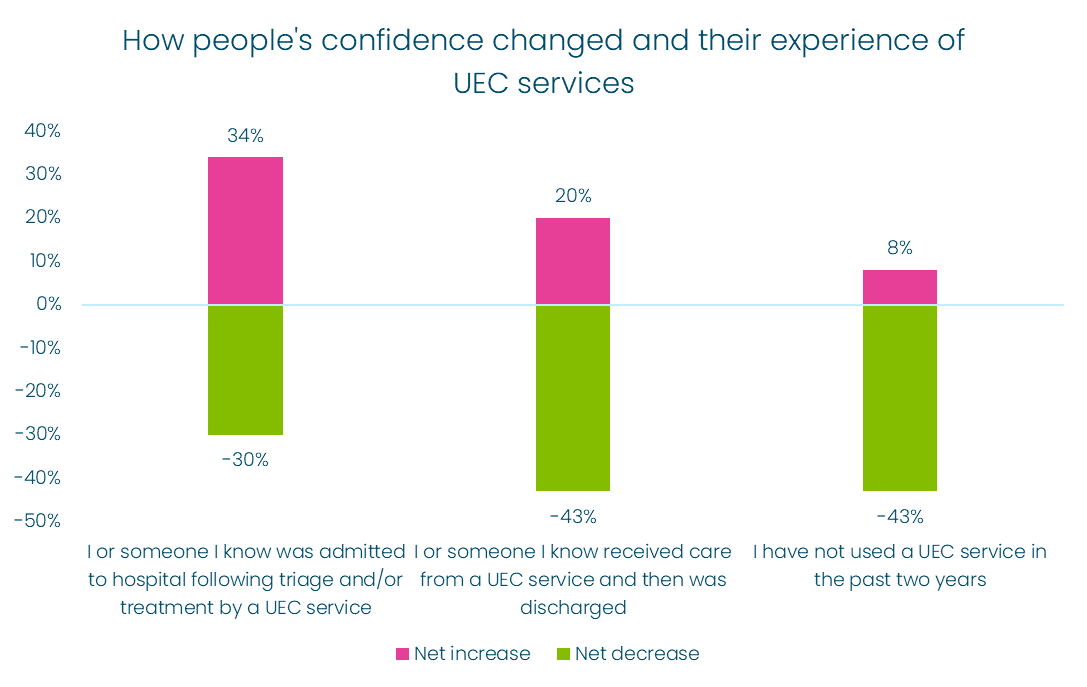
Nearly half (49%) of the people we asked had an experience of using an urgent and emergency care service, either for themselves (25%) or a loved one (24%), during the past two years.
Half of those who had an experience with an urgent care service told us that they or a loved one were then admitted to a hospital following triage and/or treatment. The other half were treated and then discharged.
What people told us:
- One in three people, or their loved ones, who used an urgent and emergency care service and were then admitted to the hospital said their confidence increased. This group was also the most likely to say their confidence increased, suggesting that the NHS has a relatively positive story to tell about how it cares for those with the most serious level of need despite current pressures.
- However, 43% of people, or their loved ones, who used an urgent and emergency care service, but were not admitted, said their confidence decreased. A considerably lower proportion of this group said their confidence increased, suggesting particular challenges for the NHS in addressing the needs of these users.
- People who did not have experience with an urgent and emergency care service were much less likely to say their confidence had increased. Just one in 12 people with no experience of an urgent and emergency care service said their confidence had increased.
Older people have lower confidence in urgent and emergency care services than younger people
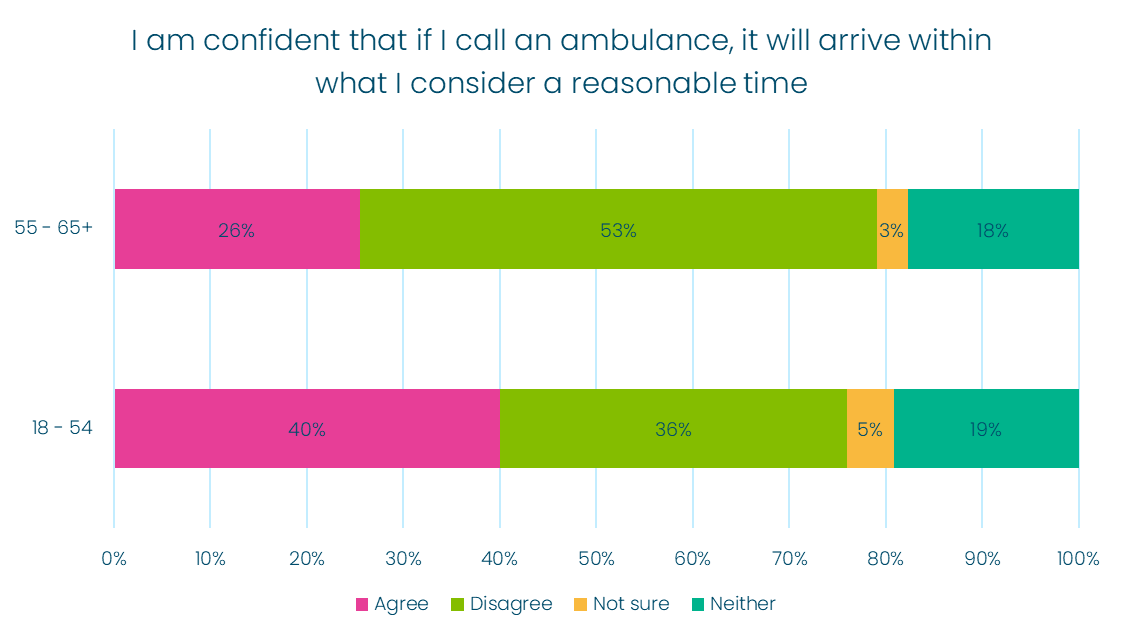
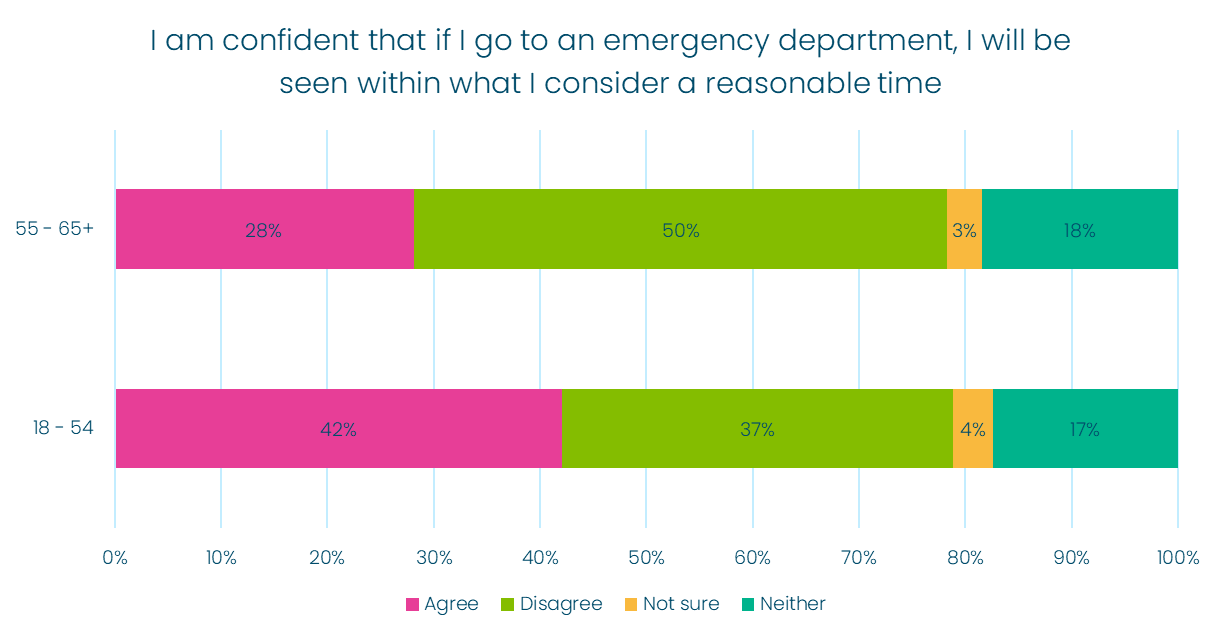
We also found that people over 55 were generally less confident that they would be seen or treated within a reasonable time than people under 55:
- Over half of older people said they were not confident that they would be seen in a reasonable time at an emergency department, nor that an ambulance would arrive in a reasonable time.
- In comparison, roughly 35% of people under 55 disagreed with the same statements.
- Older people whose confidence had changed were also more likely to say that their confidence had decreased than younger people.
- 90% of older people who told us their confidence had changed said it had decreased, compared to 60% of people under 55.
What does this mean for the NHS this winter?
The current scrutiny of urgent and emergency care services is important and is clearly an issue that concerns people.
Yet previous work has shown that whilst waiting times in A&E are important to patients, the four hour target alone does not always reflect what matters most to people. Other factors such as quick assessment, effective prioritisation of the most urgent cases and good communication are also key, and can give a clearer picture of what people can expect.
While the Secretary of State has confirmed that there are no immediate plans to change the four hour target, rolling out some additional national measures would provide people with important additional information on NHS performance, and may improve public confidence.
Some of these measures, recommended by the national review of clinical standards, include:
- How many people in A&E have their initial assessment within the target time of 15 minutes of arrival?
- How many people with the most serious conditions – such as strokes, heart attacks and sepsis – are being seen within the critical time standard?
This could help the NHS:
- Be more transparent about how urgent and emergency care services are coping with winter pressures, and build confidence that the most serious cases are getting the help they require in their hour of need.
- Set clearer expectations for those who may have to visit A&E, particularly those who may face an extended wait because of the current pressures on the system.
- Generate information and data that NHS 111 and patients could use to navigate the system better, helping people access emergency departments at less busy times or getting care via alternative services.
Downloads
If you require this briefing in an alternative format, please get in touch and let us know.
If you want to see the questions and answers from our polling in more detail you can view the data here.
